Accurately billing CPT 99221, 99222, and 99223 is essential for internal medicine providers conducting initial inpatient or observation evaluations. This guide walks you through code selection by complexity or time, documentation essentials, and key contrasts with outpatient E/M billing practices.
Guide to Codes by Complexity & Time
With E/M guideline revisions effective January 1, 2023, initial hospital (inpatient or observation) care codes now follow a dual-criteria approach—utilize either level of medical decision-making (MDM) or total time on the encounter date:
- 99221 – Straightforward or low complexity MDM — or ≥40 minutes total time
- 99222 – Moderate complexity MDM — or ≥55 minutes total time
- 99223 – High complexity MDM — or ≥75 minutes total time
The “medically appropriate” history and/or examination requirement has replaced prior mandates like “detailed” or “comprehensive” evaluations, simplifying documentation standards across these codes.
Documentation Requirements: What Must Be Captured
Initial hospital care codes require clear documentation of all three key components—unless time is being used as the billing basis. Here’s what to capture when selecting based on MDM:
- History: Document chief complaint, medically appropriate History of Present Illness (HPI), Review of Systems (ROS), and Past, Family, and Social History (PFSH) as germane to patient care.
- Examination: Record findings relevant to chief complaint and conducted exam—”medically appropriate” suffices; specific system counts are no longer mandatory.
- Medical Decision Making (MDM): Must meet two or three: problem complexity, data complexity, and risk level (straightforward/low, moderate, or high).
If instead billing by time, document total time spent (face-to-face and non-face-to-face on the encounter date), noting the specific minutes to meet thresholds.
Differences from Outpatient E/M Codes
These codes are intended for initial evaluation of patients admitted as inpatients or placed under observation. They explicitly do not apply to outpatient settings—choosing the wrong billing category could lead to denials or audits.
Quick Walk‑Through Examples
- Scenario 1 — 99221: A patient is admitted for mild dehydration. You conduct appropriate history and exam, moderate data review, and low-risk decision-making—total time is 42 minutes. Bill 99221 (time-based meets threshold).
- Scenario 2 — 99223: A patient with septic shock requires admission. You document a thorough history, exam across multiple systems, review extensive labs/imaging, and make high-risk decisions—all captured in 80 minutes. Bill 99223 (both high MDM and time exceed threshold).
Final Takeaways
Selecting the correct initial hospital care code—whether based on MDM or time—depends on accurately reflecting the complexity of patient care or total provider time invested. Documentation should explicitly denote which method is used, ensuring that history, exam, and decision-making align with the chosen level. Remember, these codes differ fundamentally from outpatient E/M codes in setting, intent, and billing utility. Consistent, precise documentation and code assignment reduce audit risk and promote appropriate reimbursement.
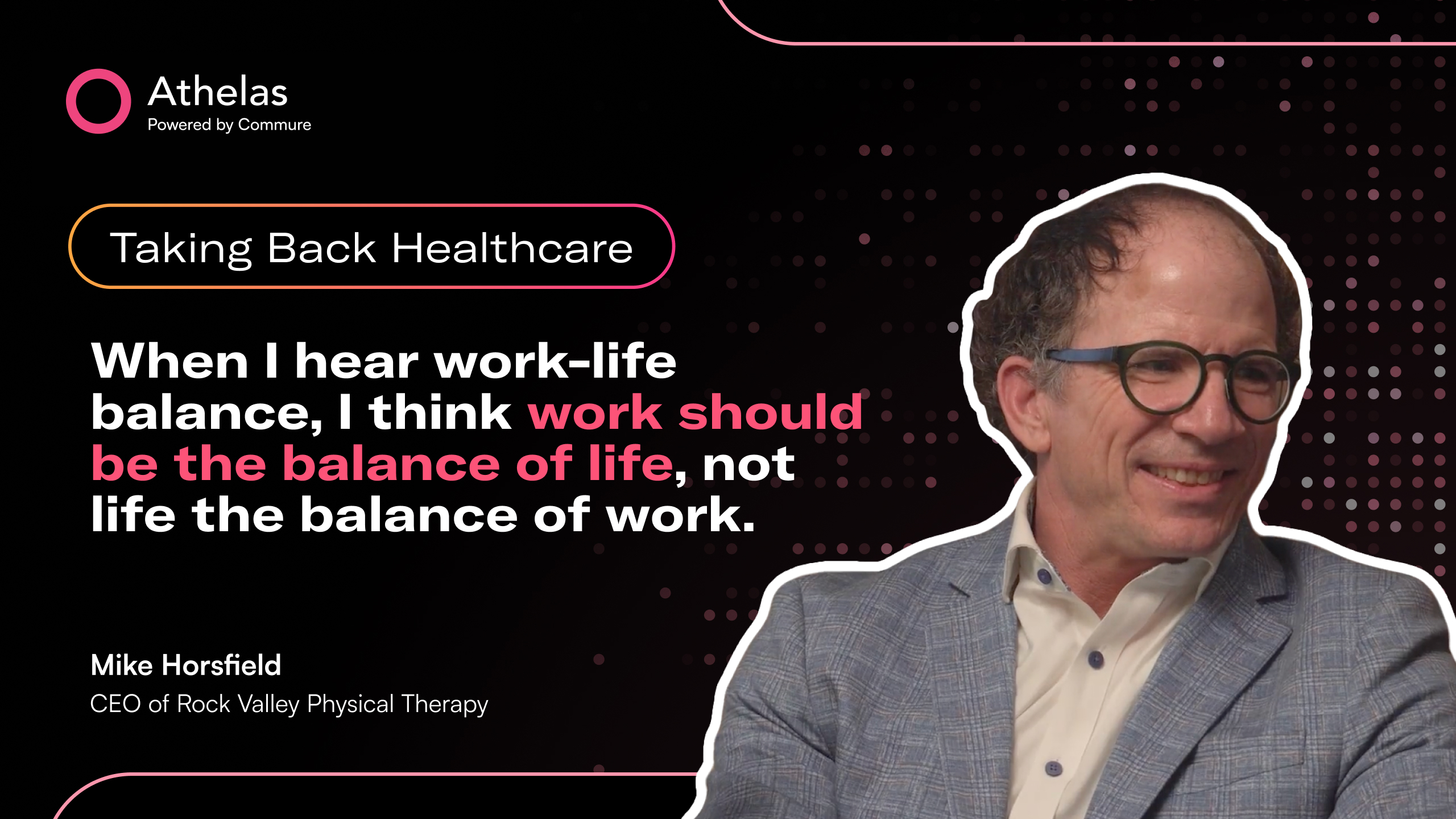
How do you bill medicaid? Improve retention without hiring?
Get ahead of 2025 CMS changes?
Schedule a demo with Athelas today to find out.